Undocumented status, ID barriers hamper vaccine access for vulnerable mothers, children in Kenya

Unvaccinated children are left exposed to preventable but potentially deadly diseases like polio, measles, tuberculosis, and hepatitis B.
When Dorcas Naikuru crossed the border from Uganda into Kenya, she was heavily pregnant, alone, and uncertain of what lay ahead.
With no official documentation and little understanding of the healthcare system, she found herself in Nairobi’s Majengo slum. With fear in her heart but hope in her hands, she began a difficult journey of motherhood in a new country, one where even accessing basic maternal care would prove to be a daily struggle.
More To Read
- Review meeting highlights barriers to immunisation, maternal health in Turkana
- How Riruta’s upgrade to Level IV hospital is transforming healthcare across Dagoreti
- Nairobi County moves to formalise and regulate childcare sector
- From free to unaffordable: Why more Kenyan women are giving birth at home again
- From hope to despair: HIV patients left behind by Kenya’s health transition
- Marsabit Senator urges Senate to resolve CHP payment delays, water project setbacks
Because she lacked documentation, Naikuru was initially too afraid to seek care at public health clinics. She feared being turned away—or worse, getting into legal trouble for not having a Kenyan ID or passport.
After giving birth in a public facility, her baby received the first routine vaccine—a small but meaningful relief. But that comfort was short-lived. When she returned for the next round of immunisations, she was asked to present valid identification. Without a Kenyan ID or passport, she was turned away. Feeling helpless and unsure of where to turn, she stopped going back. Not because she didn’t care, but because the system had closed its doors to her.
“I didn’t know what to do,” she says. “I just stayed home and hoped things would work out.”
Naikuru had heard about Community Health Promoters (CHPs) who sometimes go door-to-door offering vaccines. “Maybe when they come, I’ll be able to vaccinate my child,” she says. But no one has come to her door yet.
Unaware of the ongoing vaccine shortages or the timing of restocks, Naikuru continues to wait. Like during the polio campaigns she witnessed in the past, she hopes someone will eventually show up to help.
The problem is compounded by these frequent shortages. When vaccines are unavailable, CHPs often refer families to health facilities. But for someone like Naikuru, without an ID, even a referral leads nowhere.
“At the hospital, they ask for an ID, which I don’t have and SHA,” she explains. “And I don’t have the money to get the documents. Without them, I can’t get treatment for myself or my baby—unless I go to a private hospital, and most of the time, I can’t afford that either.”
Naikuru’s situation is far from unique. During the COVID-19 pandemic, routine birth immunisations dropped dramatically across Kenya. Since then, vaccine shortages have become the norm. Many newborns are discharged from hospitals without vital protection against diseases like tuberculosis, hepatitis B, and polio. Often, these critical vaccines are administered months later, raising serious concerns about their effectiveness and long-term impact.
Recently, after several days of shortage, the BCG vaccine and Polio were restocked in the country. But for mothers like Naikuru—still waiting, still undocumented—the barriers to access remain firmly in place.
In 2024, a single positive environmental surveillance sample was detected in Kamukunji Sub-County, Nairobi—an area that includes Majengo slum. This triggered a nationwide polio vaccination campaign. The detection was a red flag, indicating the silent circulation of the poliovirus in the community. Around the same time, four confirmed polio cases were reported in Kakuma Refugee Camp, highlighting the vulnerability of communities with low immunisation coverage.
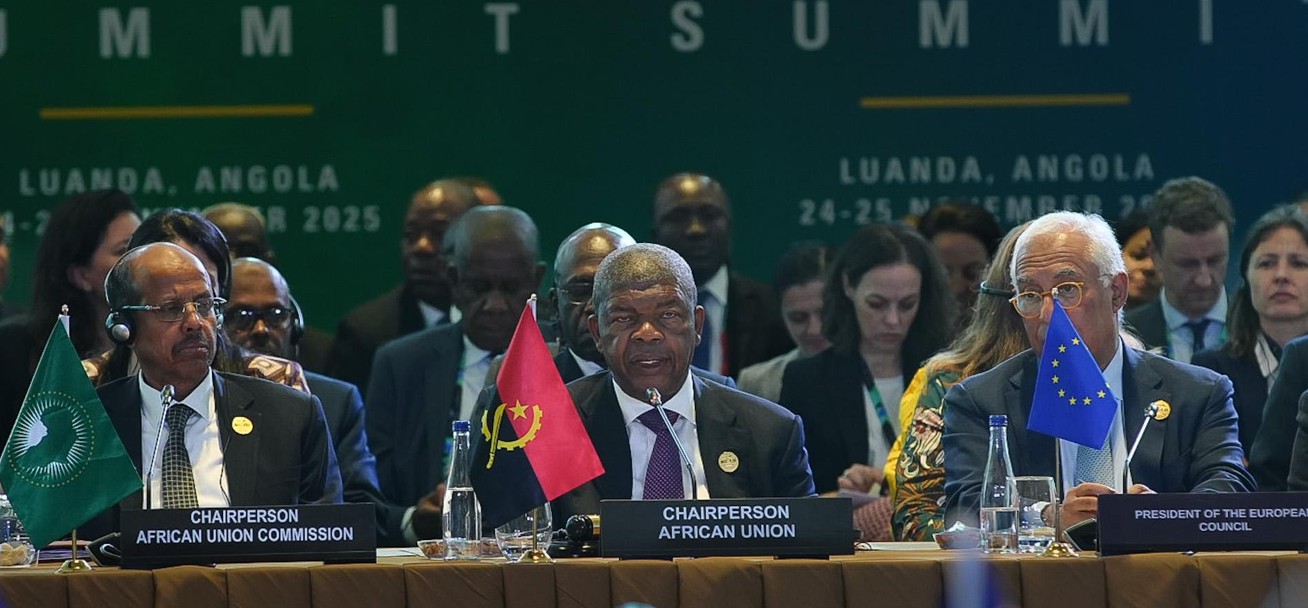
 Community Health Workers administering polio vaccine to children in Garissa County. (Photo: Issa Hussein)
Community Health Workers administering polio vaccine to children in Garissa County. (Photo: Issa Hussein)
When vaccines are not administered on time, the consequences can be severe. Unvaccinated children are left exposed to preventable but potentially deadly diseases like polio, measles, tuberculosis, and hepatitis B. Polio, for instance, can spread silently through contaminated water and food, often infecting children without immediate symptoms. By the time paralysis appears, it is too late to reverse the damage, and it signals that many more may already be silently infected.
Delays or missed immunisations not only put individual children at risk but also weaken herd immunity, increasing the likelihood of outbreaks. In densely populated urban informal settlements like Majengo, where sanitation is poor and health access is limited, even a single missed vaccination can trigger a chain reaction with far-reaching public health consequences.
Dr. Esther Mwaura, based in Nairobi, emphasises the critical importance of timely vaccinations, especially in vulnerable communities. She explains that failing to vaccinate children doesn’t just leave them susceptible to specific diseases—it can weaken their overall immunity and make them more prone to frequent illnesses, particularly in epidemic-prone areas or places with poor sanitation and unsafe environments.
“When a child is not vaccinated, it becomes much harder to monitor their health milestones, which are often early indicators of underlying or serious conditions. During routine immunisation visits, healthcare workers don’t just administer vaccines—they also assess the child’s growth, development, and general well-being. These visits are crucial opportunities to catch problems early, from nutritional deficiencies to developmental delays.”
In areas like Majengo slum, where children face multiple health risks due to overcrowding, poor water quality, and limited healthcare access, missing vaccinations increases their vulnerability on several fronts. Without regular contact with healthcare providers, many children miss out on essential screenings and preventive care, allowing treatable conditions to go unnoticed and worsen.
“When children remain unvaccinated, they not only risk their own health but also contribute to the continued circulation of infectious diseases within the community. This puts everyone, especially infants and the immunocompromised, at greater risk of outbreaks.”
In 2020, the COVID-19 pandemic disrupted health systems across the world, and childhood immunisation services were among the hardest hit. Globally, 23 million children missed out on basic vaccines through routine immunisation programmes—the highest number recorded since 2009. Of those, an estimated 17 million children did not receive even a single dose of any vaccine that year, leaving them completely unprotected and heightening the risk of outbreaks.
The consequences of this disruption were severe. Diseases once on the brink of eradication made alarming comebacks. For instance, over 60 million children missed their measles vaccinations globally, contributing to significant surges in measles outbreaks in several regions. Missed vaccinations also increased the threat of polio, diphtheria, and other preventable illnesses, especially in overcrowded or under-resourced communities.
In Kenya, the situation mirrored global trends. The pandemic led to a sharp decline in routine childhood immunisation coverage. Thousands of children missed critical vaccines in 2020. In some counties, the administration of the third dose of the diphtheria, pertussis, and tetanus vaccine (DPT3)—a key indicator of immunisation coverage—dropped by as much as 25 per cent. Although the government later launched catch-up campaigns, reaching an estimated 3 million children.
The implications of missed immunisations go far beyond the individual child. Unvaccinated populations reduce herd immunity, making it easier for diseases to spread.
On June 6, it was reported that 12 of Kenya’s 47 counties have completely run out of vaccines, marking the second time this year the country has faced such shortages, the Ministry of Health confirmed in a statement released on Friday by Principal Secretary Ouma Oluga. The Ministry highlighted that the nation is currently experiencing critically low stock levels of several essential vaccines.
On Thursday, Health Cabinet Secretary Aden Duale flagged off a major shipment of life-saving vaccines, signalling renewed momentum in Kenya’s child immunisation efforts.
The country has received over six million doses—3 million of the Bacille Calmette-Guérin (BCG) vaccine, which protects against tuberculosis, and 3.2 million doses of the Oral Polio Vaccine (OPV). This delivery, made in collaboration with UNICEF and other immunisation partners, comes amid recent worries about stockouts of critical childhood vaccines.
“This consignment was made possible thanks to the swift and commendable action of the National Treasury, and we are deeply grateful for their rapid allocation of resources,” said Duale. “I urge all county health teams to prioritise vaccine distribution to restore full immunisation coverage nationwide.”
He called on parents and guardians to take their children to the nearest health facility for any missed or upcoming vaccinations. “These vaccines are now available, and this is the time to ensure every child is protected against deadly but preventable diseases,” he said.
Top Stories Today